Endometriosis can take years and requires surgery to diagnose. Researchers say they are close to a solution

Before getting that diagnosis, Balducci said she spent nearly two decades of her life living with menstrual cycles so painful she’d have to miss work or school.
“I’ve been to the [emergency room] because the pain was so bad sometimes I thought, ‘This can’t just be cramps. This has to be my appendix bursting,'” Balducci told “Good Morning America.” “I consistently was told that my [period] pain was normal. Nobody mentioned the word endometriosis once.”
It was only last year, as Balducci was starting the process of freezing her eggs, that she said a fertility doctor told her she should see a specialist for her pain.
Once she saw a specialist who told her she likely had endometriosis, Balducci had to undergo laparoscopic surgery, as it is currently the only way to diagnose the disease.
“It’s really invasive … and the recovery is very intense,” Balducci said of the surgery. “And the diagnosis and the surgery, for many, is a step because there is mystery around if the endometriosis is going to grow back, and if the pain is even going to go away.”
Researchers believe that endometriosis — a disease where the tissue forming the inner lining of the uterus is found outside of the uterus such as within the fallopian tubes, ovaries, bladder and intestines — affects more than 6 million women in the U.S. and as many as 200 million women worldwide.
Though it is one of the most common gynecological diseases, according to the National Institutes of Health, getting a diagnosis is often similar to Balducci’s experience: long and painful.
On average, women wait as long as seven to 10 years for a diagnosis, according to Christine Metz, Ph.D., head of the laboratory of medicinal biochemistry and a professor in the Institute of Molecular Medicine at the Feinstein Institutes for Medical Research in New York.
Metz said the delay can be due to everything from women being told their menstrual pain is normal, as in Balducci’s case, to the symptoms of endometriosis — painful menstrual cramps, chronic lower back and pelvis pain, pain during and after sex, bleeding or spotting between periods and digestive problems like diarrhea, constipation, bloating and nausea — being misdiagnosed and treated as gastrointestinal issues.
In many cases, the delay happens, she said, because patients are either not referred for diagnostic surgery, or are hesitant to undergo such an invasive surgery in order to be diagnosed.
“Endometriosis can only be definitively diagnosed through laparoscopic surgery, and that means a small camera is inserted into the abdominal cavity to look for endometriosis lesions,” Metz said. “The suspected lesions that they find during this scoping procedure are removed and then analyzed for the presence of endometrial-like cells.”
Metz said that in her own experience, she has seen patients who have gone as long as 20 years without a diagnosis of endometriosis.
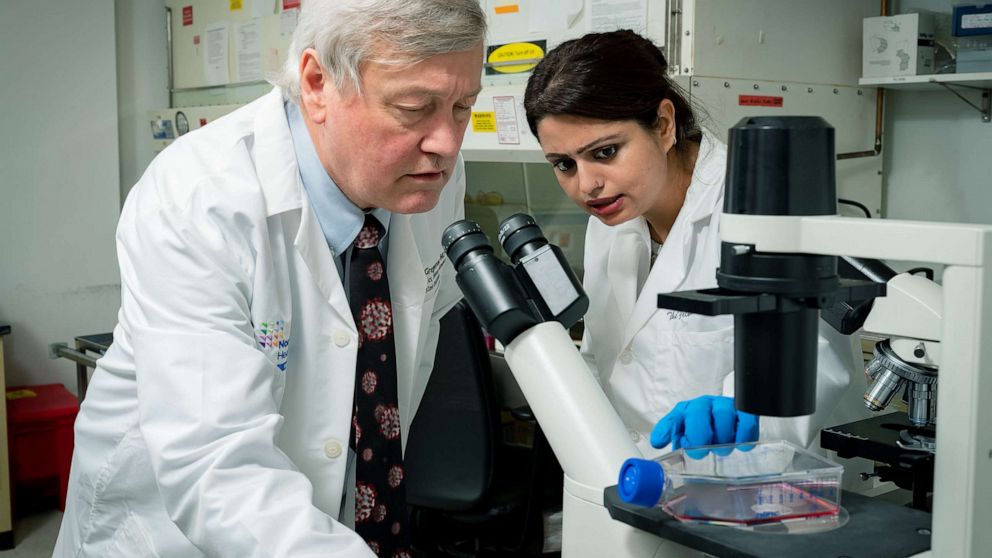
For the past six years, Metz has worked to find a way to diagnose endometriosis that does not require surgery.
She and her research partner, Dr. Peter Gregersen, a rheumatologist and genetics researcher, believe they have found the answer in something that comes monthly for menstruating women: menstrual blood.
“Scientifically, it makes a lot of sense because the lesions that are found in the pelvic cavity contain the same cells that are found in menstrual blood,” Metz said. “And we believe that if you were healthy, most of that tissue and material would be removed.”
So far, more than 2,400 women around the world have taken part in the study.
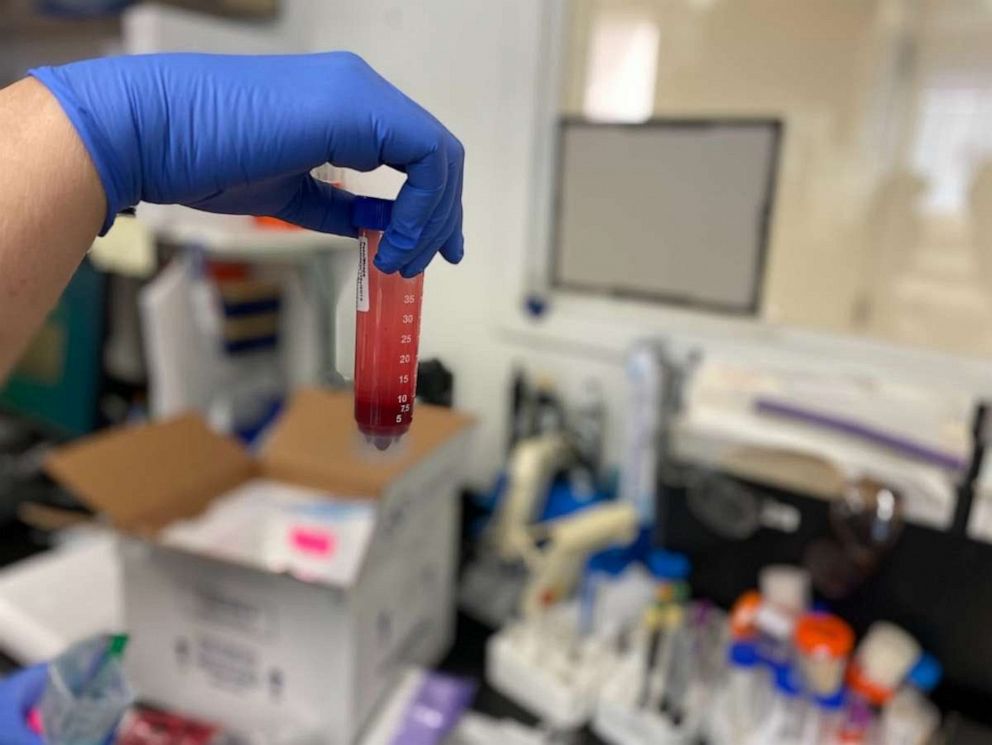
The menstrual blood samples are collected through menstrual sponges that Metz and Gregersen created as a way to collect the sample without any type of insertion, a request that came from participants, according to Metz. The researchers have also worked, she said, to make the diagnostic test “reasonably priced” so it is not cost-prohibitive once it hits the market.
By collecting just a small amount of menstrual blood on the sponge and then analyzing it, Metz said they have been able to document differences in the menstrual blood of people with endometriosis.
Late last year, Metz and Gregersen began a new clinical trial focused on people who are preparing to undergo laparoscopic surgery. The goal of the trial is to see if menstrual blood analysis can be used as a way to screen people for endometriosis, which would help people know more definitively that they could benefit from surgery.
“We hope to finish the trial by the end of this year or the beginning of next year and submit materials to the [U.S. Food and Drug Administration], so that we could get an FDA approval for either a diagnostic for endometriosis or a screening tool,” Metz said.
Endometriosis currently has no known cause, but Metz said by studying menstrual blood, she and Gregersen have been able to start unlocking some of the mysteries of how this common disease starts.
There is no known cure for endometriosis, but treatment options include medications and/or surgery, including the medication Orilissa, which has been specifically studied and marketed for the treatment of endometriosis pain.
Metz said that due to a “frustrating” lack of research, doctors and researchers do not yet know what it would mean for women to be diagnosed with endometriosis soon after their first-ever menstrual cycle instead of years or decades later.
“We haven’t even been able to study whether early diagnosis will impact anything, because it’s never been studied in any organized way,” Metz explained. “We don’t know whether early diagnosis with the current therapies will even do anything.”
Through their years of research on menstrual blood, Metz said she and Gregersen have discovered it may help with more than endometriosis, and instead be more of a window into a woman’s overall uterine health.
“Nobody studied menstrual blood with respect to endometriosis, or any uterine condition, prior to our work,” Metz said. “It was never used to understand women’s health.”
In the future, Metz said she hopes collecting a menstrual blood sample will be a routine part of a gynecological exam.
“We believe it was a completely neglected biological sample, perhaps related to the ‘yuck factor’ associated with it,” Metz said of menstrual blood. “We have to dispel all of the negative discussion of being afraid to discuss periods and menstruation … We’re not afraid to talk about our leg pain or arm pain or our tooth pain, but somehow we’ve been quieted.”